T he word gout may make you think of overweight Victorian-era royalty with overly rich diets. But this common form of inflammatory arthritis, which leads to pain and swelling in one or more joints—especially in the lower body—affects people even in the modern era. In fact, more than 9 million adults in the U.S. have been diagnosed with the disease, which occurs when the body produces too much uric acid or the kidneys don’t excrete enough.
That surplus forms crystals in and around joints, eventually causing flares or attacks. “People with high levels of uric acid can be accumulating crystals and damage to the joints for years before they have their first gout attack,” says Larry Edwards, MD, a professor of medicine at the University of Florida.
Gout is on the rise, says John FitzGerald, MD, a professor of medicine at the David Geffen School of Medicine at UCLA and an author of guidelines from the American College of Rheumatology (ACR) about gout management.
A genetic predisposition, diabetes, kidney disease, and other health problems may increase the chance of developing it. “The growing number of people with metabolic syndrome and obesity is increasing the risk of gout,” says FitzGerald, adding that some of the treatments for the conditions mentioned above may also raise the risk.
When Gout Strikes
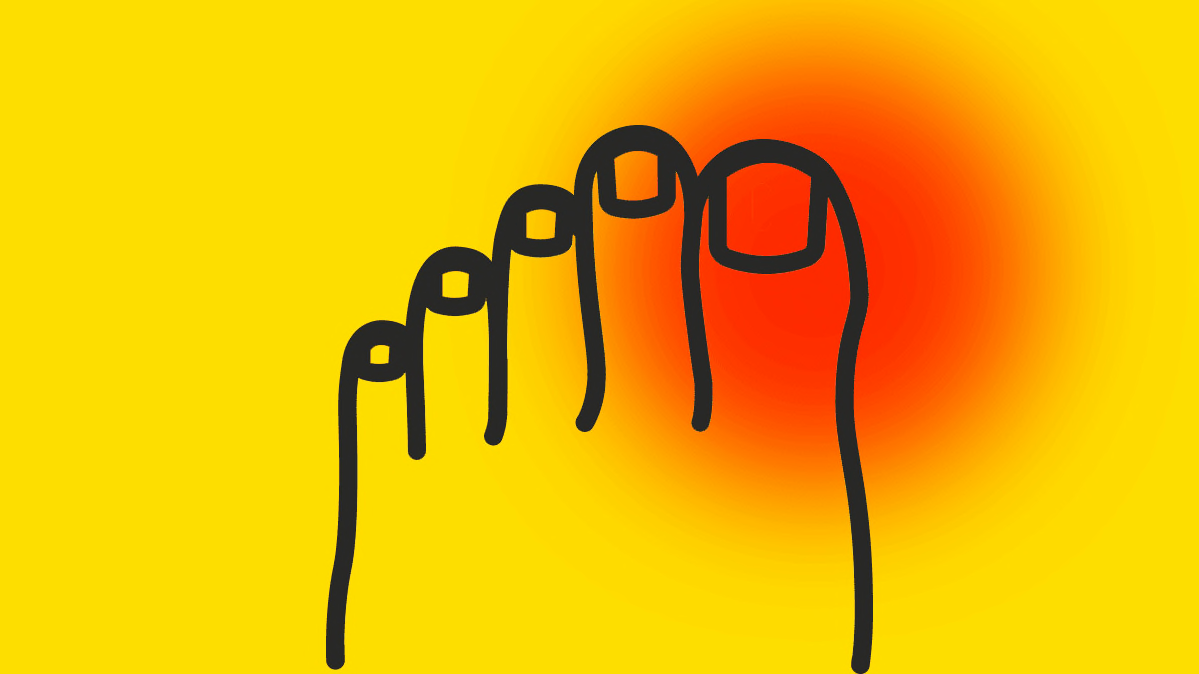
An acute gout attack, which most often strikes one of the big toes, is hard to dismiss. “Gout attacks are intensely strong and come on quickly,” FitzGerald says. “They manifest as a red, inflamed joint that is difficult to move or even put weight on.”
Sufferers are often in so much pain that they end up in an emergency room, so get medical help right away if you experience such symptoms. Your doctor can confirm or rule out gout by checking fluid from the affected joint for crystals and by measuring uric acid levels in your blood.
The Right Treatment Plan
Over-the-counter medications such as ibuprofen (Advil or Motrin), prescription anti-inflammatory drugs like colchicine (Colcrys or Mitigare), and prescription steroids like prednisone (Rayos) can help reduce joint pain and swelling during an acute attack or flare.
Long-term, your doctor may recommend urate-lowering therapy (ULT), which means taking medications such as allopurinol (Zyloprim or Lopurin) and febuxostat (Uloric) daily. “There is the possibility of future damage to your joints if you don’t control it,” says Stanford Shoor, MD, a clinical professor of medicine and rheumatology at Stanford University.
ACR recommends ULT if you have tophi (crystal nodules on joints) or evidence of joint damage, or if you’ve had two or more attacks in a year. But “whether or not you start ULT after one attack depends a bit on how much we think you’re going to have future attacks,” FitzGerald says. “If you don’t have kidney disease or very high uric acid levels, it may be years before you have another attack, and you might not want to go on daily therapy.”
The standard of care generally calls for what’s called “treat to target,” starting with a low dose of ULT and adjusting it until your uric acid levels drop to a specific level. Newer ACR guidelines strongly recommend treatment that keeps uric acid concentrations below 6 mg/dL, which is low enough to keep the acid from crystallizing.
But studies suggest that only about one-third of people with gout are receiving ULT. “Patients often don’t understand the difference between treating flares and prevention,” says Shoor, making them less willing to take a daily drug. And ULT requires patience. “It takes time to lower uric acid levels—sometimes up to six months—and your flares might get worse before they get better,” FitzGerald says.
Can Diet Make a Difference?
Your doctor may recommend that you limit foods that may hike uric acid levels. That includes organ and red meats, shellfish (high in the compound purine), alcohol (especially beer), and sugar and high-fructose corn syrup.
According to the ACR, purine-rich vegetables like mushrooms and spinach should be fine, and low-fat dairy foods may help lower uric acid levels. But even with a gout-preventing diet, “most people see, at best, a modest decline in uric acid levels,” Shoor says. So if you’re on ULT, sticking to your regimen is key.
https://www.consumerreports.org/arthritis/how-to-treat-gout/
No comments:
Post a Comment