From krdo.com
Psoriatic arthritis is an autoimmune condition that causes joint inflammation, skin symptoms, and pain. People searching for psoriatic arthritis prescriptions are often looking for detailed information about medication options, their effectiveness, potential side effects, and ways to manage costs.
This guide from SaveHealth, a prescription discount/savings card website, explores the most commonly prescribed medications for psoriatic arthritis, including DMARDs, biologics, and NSAIDs, while highlighting considerations for effectiveness, safety, and cost.
Ray Geiger // Shutterstock
How Psoriatic Arthritis Medications Work
Medications for psoriatic arthritis aim to reduce inflammation, slow disease progression, and relieve pain. They work through different mechanisms depending on the drug class.
Major medication categories:
- DMARDs (Disease-Modifying Anti-Rheumatic Drugs): These slow disease progression and prevent joint damage. Examples include methotrexate and leflunomide.
- Biologics: Target specific components of the immune system to control inflammation. Examples include Skyrizi and Humira.
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Provide temporary relief from pain and stiffness without altering disease progression. Examples include naproxen and celecoxib.
- Corticosteroids: Offer rapid symptom relief during flare-ups but are generally used short term.
- PDE-4 Inhibitors: Commonly known as phosphodiesterase-4 inhibitors, these drugs work by blocking the PDE-4 enzyme which ultimately helps to lower inflammation in the body. A frequent used example is Otezla.
Top Psoriatic Arthritis Medications
The following medications are among the most commonly prescribed for psoriatic arthritis. They include both traditional and newer therapies.
DMARDs
- Methotrexate: Often first-line therapy for psoriatic arthritis. It slows joint damage and inflammation.
- Leflunomide: Useful for patients who cannot tolerate methotrexate.
- Sulfasalazine: Reduces joint inflammation and can improve skin symptoms.
Biologics
- Skyrizi (risankizumab): Targets interleukin-23, reducing inflammation and improving both joint and skin symptoms.
- Humira (adalimumab): TNF inhibitor that helps reduce pain and swelling.
- Enbrel (etanercept):TNF inhibitor that can slow joint damage and improve quality of life.
- Stelera, Imuldosa, Otulfi, Pyzchiva, Selarsdi, Steqeyma (ustekinumab): Targets IL-12 and IL-23 to control inflammation.
NSAIDs
- Naproxen: Reduces pain and stiffness.
- Celecoxib: Offers pain relief with reduced gastrointestinal risk compared to traditional NSAIDs.
Corticosteroids
- Prednisone: Provides rapid relief during flares but is not intended for long-term use due to side effects.
Psoriatic Arthritis Medication Comparison
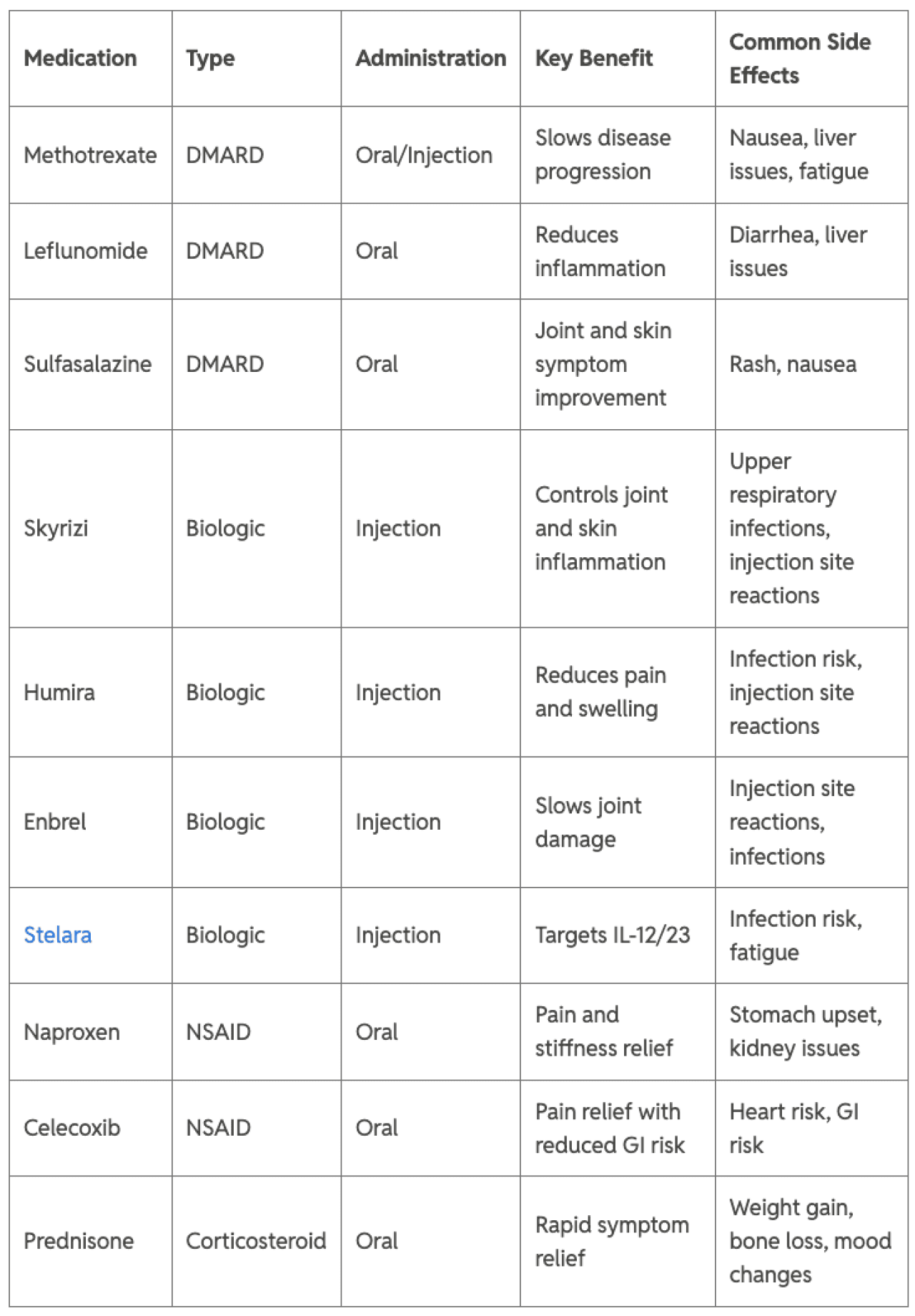
SaveHealth
Otezla PDE-4 inhibitor Oral Significant joint relief Nausea, decreased in 16 weeks appetite, weight loss, anxiety, insomnia.
Common Side Effects of Psoriatic Arthritis Medications
Side effects vary depending on the type of medication and individual response.
DMARDs
Biologics
- Increased risk of infections
- Injection site reactions
- Upper respiratory infections
NSAIDs
- Stomach upset
- Kidney issues
- Increased bleeding risk
Corticosteroids
- Bone loss
- Weight gain
- Mood changes
PDE-4 inhibitors
- Gi side effects (Nausea, diarrhea, decreased appetite, abdominal pain, weight loss)
- Headache, dizziness, insomnia, anxiety, nervousness
- Infections (upper respiratory infections)
Choosing A Psoriatic Arthritis Medication
Selecting the appropriate psoriatic arthritis medication requires balancing effectiveness, side effect tolerance, convenience, and cost.
Factors to consider:
- Severity of joint and skin symptoms
- Past medication response
- Risk of side effects
- Administration preference (oral vs injection)
- Insurance coverage and out-of-pocket cost
Tips for Managing Psoriatic Arthritis Medication Costs
Psoriatic arthritis medications, particularly biologics and DMARDs, can be costly. Patients can reduce expenses by:
- Comparing pharmacy prices
- Considering generic options for DMARDs
- Exploring manufacturer savings programs
- Reviewing insurance co-pay assistance
- Planning prescriptions to avoid gaps in therapy
Even small monthly savings can make a significant difference for long-term disease management.
Psoriatic Arthritis Medications & Prescriptions
Psoriatic arthritis management involves a range of medications, including DMARDs, biologics, NSAIDs, and corticosteroids. Understanding options like Methotrexate, Leflunomide, Sulfasalazine, Skyrizi, Humira, Enbrel, Stelara, Naproxen, Celecoxib, and Prednisone helps patients select effective therapies for their condition. Working closely with a healthcare provider while considering effectiveness, safety, and affordability can optimize long-term outcomes.

